Esophageal varices often occur in people with liver disease, symptoms are poor but complications are very unpredictable.
Esophageal varices develop when normal blood flow to the liver is blocked by a blood clot or scarring in the liver. The condition can be fatal due to serious complications.
Esophageal veins are small and have thin walls that cannot hold large amounts of blood. Therefore, stagnant blood flow can cause the veins to dilate and rupture. Esophageal varices can be dangerous, even fatal. Therefore, any patient suspected of having esophageal varices must go to the hospital immediately for examination, diagnosis and timely treatment.
1. Causes of esophageal varices
– Cirrhosis is the most common cause of esophageal varices. Of those with cirrhosis, 30% have varices with a blockage in blood flow to the liver. In the first year after diagnosis, 5% of small varices and 15% of large varices bleed.
– Portal hypertension is a complication of cirrhosis that occurs when scar tissue blocks the flow of blood around the liver. This leads to high blood pressure in the portal vein, which is the tube that carries blood from other organs to the liver.
– If blood flow around the liver is restricted, the body will increase blood flow through veins in the stomach or esophagus. When blood flow through them increases too much, it can cause varices.
– Rare causes of esophageal varices include Budd-Chiari syndrome and schistosomiasis. Budd-Chiari syndrome causes the veins in the liver to become partially blocked. Schistosomiasis can invade the blood vessels, causing the veins to dilate.
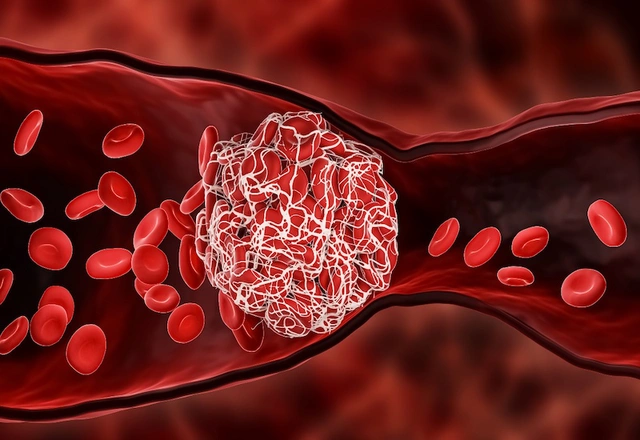
Blood clots in esophageal veins are a cause of varicose veins.
2. Symptoms of esophageal varices
Esophageal varices have poor symptoms, often detected when bleeding occurs. Signs and symptoms of esophageal bleeding are vomiting blood (little or massive) or passing black stools. These manifestations appear when the veins have dilated to the maximum level, causing perforation or rupture of the veins, causing bleeding. The patient has unusually pale skin; Constant fatigue; Shortness of breath; Fainting or dizziness, …
Esophageal varices can only be detected through esophagography (drinking barite or examining the esophagus with a flexible endoscope).
3. Complications of esophageal varices
The most dangerous complication of esophageal varices is bleeding. When this condition occurs, there are many other potential risks, such as when the patient bleeds too much, they are susceptible to shock and in the case of not being given emergency care and timely treatment, the mortality rate is very high.
According to statistics, up to 50% of people with cirrhosis have complications of esophageal varices. The risk of bleeding complications is very high, the rate of recurrent bleeding is high after treatment.
4. Diagnosis of esophageal varices
Diagnosis of liver disease requires a combination of many different aspects and techniques including: Symptoms; Medical history, clinical examination; Blood test results and liver biopsy if necessary.
People with cirrhosis should regularly check for esophageal varices by performing techniques such as endoscopy or computed tomography (CT Scan).
5. What to do when having esophageal varices?
If there are symptoms of fatigue, loss of appetite, pain in the liver area, etc., the patient needs to go to the hospital for examination to know their health status, from which timely treatment measures can be taken.
In case the patient vomits blood, the esophageal vein may rupture, and must be quickly taken to the hospital for emergency treatment to stop the bleeding.
In general, the primary goal of treating esophageal varices is to stop bleeding. Esophageal bleeding can be life-threatening, so the best way to avoid this risk is to proactively prevent and control liver disease.





